Peyronie’s disease can be a complex and sensitive condition requiring expert evaluation and treatment. We provide individualized care with the full range of medical and surgical treatments in a comfortable and private setting.
MetroWest Urology is a national center of excellence for the treatment of Peyronie’s Disease, serving patients from the greater Boston area and beyond. Peyronie’s disease can be a complex and sensitive condition requiring expert treatment. We provide highly individualized care with the full range of medical and surgical treatments in a comfortable and private setting.

Peyronie’s results from deposition of collagen (scar-like tissue) called a “plaque” in the lining around the erectile bodies. Red arrows indicate potential sites for plaque formation. The plaque can be on the top (dorsum), bottom (ventral), or in between the erectile bodies (septal). Adapted from
Campbell-Walsh Urology Ninth Edition
Peyronie’s Disease refers to a curve, bump, or indentation that develops in the penis. Peyronie’s is the result of scar-like or “plaque” that forms in the membrane that surrounds the erectile bodies in the penis (called the “tunica albuginea”.) The plaque is a dense deposit of scar-like tissue (called “collagen”) that prevents part of the penis from expanding during an erection. As such, men may feel a sense of contracture or restriction to their erection and may develop a curve or indentation with the erect penis. This may interfere with sexual function, or in some cases make satisfactory sexual function impossible.
Peyronie’s is not a cancer. It is related to a class of medical problems called autoimmune disorders which include asthma and rheumatoid arthritis. Peyronie’s is the penile manifestation of Dupuytren’s contracture, which is a similar disorder of the palms of the hands caused by abnormal deposition of collagen scar-like tissue. While Peyronie’s disease may severely affect sexual function, it does not pose a threat to a man’s overall health.
Peyronie’s disease is not commonly discussed, but it is much more common than most men realize. Reports of penile curvatures exist from ancient times, but the disorder was first described in detail by De La Peyronie, a French physician in the 17th century. Most modern studies suggest that up to 3-7% of all men will develop Peyronie’s.
Fortunately, our understanding of Peyronie’s disease is far deeper than in the past and we now have successful and non-invasive treatment options for many men.
Peyronie’s Disease and Erections
The plaque (collagenous scar-like tissue) that forms in the penis with Peyronie’s and its effect on erections can vary greatly from one man to another. Sometimes, the plaque is relatively soft but in other cases can be highly calcified and, rarely, it can even resemble bone. Most plaques start out soft and may be tender, but over time harden into a defined shape. During this process, the shape of the erection can change, until it eventually stabilizes. The size, shape, location, and consistency of the plaque all impact the shape of the erection. The shape of the penile erection may also change with a partial erection compared to a 100% full erection.
The plaque can occur anywhere along the course of the membrane surrounding the two erectile bodies of the penis (tunica albuginea), and sometimes between or inside the erectile bodies. Most men with Peyronie’s have a single plaque, but some may have two or more. A curve or indentation can develop in any direction and in severe cases can be greater than 90 degrees. Many men with Peyronie’s may also notice a significant loss of length of the erection.
It not unusual for men to have Peyronie’s plus some degree of erectile dysfunction. This may be because the underlying environment that causes Peyronie’s disease may also lead to erectile dysfunction. Another theory is that decreased pressure in the erectile bodies may predispose a man to develop Peyronie’s. If erectile dysfunction is present, even to a minor degree, then the workup and treatment of Peyronie’s disease often involves workup and treatment of erectile dysfunction.
Peyronie’s Disease and Pain
Early in the development of Peyronie’s the plaque or scar-like tissue can be tender, both at rest and with sexual activity. This tenderness inevitably resolves, but this may take 6 months or longer as the plaque stabilizes into a firm area within the penis. In some cases, men may still have pain due to curvature or restriction of expansion of the penis during erection. Partners may have pain due to severe curvature of the penis during the erection.
What Causes Peyronie’s Disease?
In some cases, severe trauma to the erect penis can lead to a small tear or injury in the tunica albuginea (the membrane surrounding the erectile bodies of the penis). However, many cases of Peyronie’s are not associated with a specific traumatic episode. Instead, changes in overall health and the biologic environment of the penis can make it so that Peyronie’s can occur due to microtrauma from routine activity.
Men may be more likely to develop Peyronie’s if they have a family member with Peyronie’s or Dupuytren’s contracture. Men who develop scar-like tissue elsewhere in the body, such as keloids, and men who have other autoimmune disorders may be more likely to develop the environment necessary to develop Peyronie’s. Men may also develop Peyronie’s due to hormonal problems such as low testosterone, which can lead to a thinning of the membrane around the erectile bodies of the penis. General health problems such as diabetes and high cholesterol are thought to contribute to Peyronie’s, although this is not always the case. In some studies, there is an association with depression and possibly with psychiatric medications.
Peyronie’s disease may develop after treatment for prostate cancer with surgery or with radiation. In some studies, 16% of men who had their prostate cancer developed Peyronie’s. However, the true rate of Peyronie’s after prostate cancer treatment may be even higher as many men who are treated for prostate cancer do not seek help for sexual dysfunction. However, nearly all men who have been treated for prostate cancer are candidates for treatments that can restore satisfactory sexual function.
Workup for Peyronie’s Disease
The workup for all patients with Peyronie’s disease involves a history and physical exam. In some cases, the Peyronie’s disease is minor and does not interfere with sexual function. If there are other symptoms, we may check blood labs to identify an underlying problem, such as low testosterone. In the absence of bothersome or concerning signs and symptoms, men may not require further workup or treatment.
For men who have Peyronie’s disease that interferes with sexual activity, or for men who have both Peyronie’s and Erectile dysfunction, further workup is usually indicated. This involves a blood test for male hormones (including testosterone). We offer expert phlebotomy services in our office and the most important lab results can usually be obtained within 15 minutes.
The workup also involves a penile ultrasound and erection study. The degree and location of curvature or deformity can be measured in preparation for potential treatment. At the same time, the ultrasound can be used to study the speed that blood flows through the penile arteries (Doppler study). This can be used to evaluate the ability of the penile arteries to function plus the ability of the penis to trap blood in order to achieve an erection.
Medical Treatment Options
Oral and Topical Treatments
Throughout history, many pills, herbs, and vitamins have been proposed as treatments for Peyronie’s. Unfortunately, most of oral therapies have been shown not to be effective at treating Peyronie’s. Similarly, several topical salves and ointments have been tried, but these have all been shown to be ineffective. Nonetheless, in some cases, oral medications may help relieve the tenderness that some men feel early in the Peyronie’s course.
Intralesional (Injection) Therapy

Intralesional (injection) therapy with Xiaflex® or Verapamil can be effective for many men with Peyronie’s. Treatment should be individualized and performed by an experienced specialist. Image obtained from peyronies-disesase.xiaflex.com
The main form of medical treatment is called “intralesional” therapy. This involves the physician injecting medication directly into the plaque (the firm collagen scar-like that restricts the penile). Before the injection, the penis is made numb using an injection of lidocaine into the nerves at the base of the penis. The process of injection is very important to achieving good results and must be individualized and performed by a specialist. Generally, the patient undergoes several treatment sessions in combination with modeling or molding of the plaque. Modeling of the plaque should also be done at home in order to achieve the best results, regardless of the technique for intralesional injection or the medication that is used.
Xiaflex® (clostridial collagenase) is the only FDA approved medication for the treatment of Peyronie’s disease. Injections of Xiaflex are performed in the office twice a week, every six weeks. The Xiaflex medication can help break down the collagen that makes the scar-like and provide an opportunity to remodel the plaque and regain elasticity in that part of the penis. As such, it can be an effective and minimally invasive treatment for many patients with Peyronie’s disease. Since Xiaflex is an active biologic medication, it can lead to bruising and swelling that can be significant and bothersome, but temporary. In expert hands and following protocol, bruising can be kept to a minimum and permanent problems are rare.
Xiaflex is typically used after the plaque has stabilized. Xiaflex does not treat calcified areas of plaque. In some case, verapamil is injected instead of Xiaflex. Verapamil injections are typically performed every 2-3 weeks. In general, verapamil is not as effective as Xiaflex, but verapamil injections are very well tolerated and can be used for calcified and difficult to treat Peyronie’s lesions.
Historically, several other medications have been used as intralesional injections, but these have largely been supplanted by Xiaflex and verapamil. Interferon has been shown to be effective in a small subset of patients who are treated early in the development of Peyronie’s. However, it is an expensive therapy that has systemic side effects and is rarely used.
Traction Therapy
The erectile bodies of the penis are meant to be elastic and grow with an erection. With Peyronie’s there is a loss of elasticity in a specific part of the penis. Furthermore, many men with Peyronie’s OR erectile dysfunction – especially those who men who also have diabetes – may experience a loss of elasticity along the entire penis.
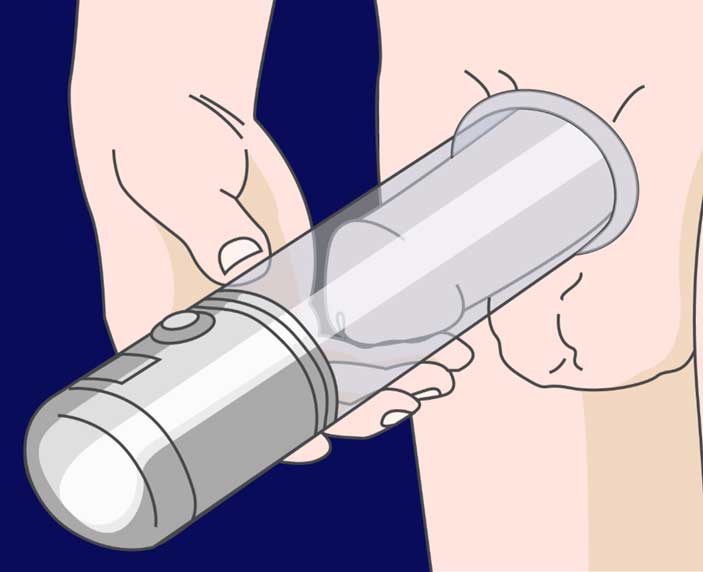
Vacuum erection devices can be used to help regain elasticity in the penis, which is lost due to Peyronie’s, Erectile Dysfunction, or Diabetes. Speak with your physician before using these devices as injury can result, particularly if patients are also undergoing intralesional therapy.
Traction therapy involves placing the penis on traction in order to help regain elasticity. There are several commercially available devices for penile traction, and vacuum erection devices can also be used to provide traction. Regular use of these devices can help to a minor degree with length lost during Peyronie’s disease or as a result of global contraction of the erectile bodies. While many of these devices are available without a prescription, they should be used under the instruction of a physician in order to avoid injury. Your urologist can also prescribe additional medications and therapies that can work in conjunction with traction therapy in order to help regain lost length.
I some cases, it is appropriate to use traction therapy in addition to intralesional therapy to help treat Peyronie’s. This should be done according to individualized instruction by your urologist as improper timing of use, especially with Xiaflex therapy can lead to severe bruising and in in some cases permanent injury.
Surgical Treatment Options
Surgical treatment for Peyronie’s disease is generally reserved for patients with severe curvature or deformity, for men who do not respond to or do not wish to undergo intralesional therapy, and for men with both Peyronie’s and erectile dysfunction.
For men who have good erectile function, a “plication” procedure can be performed to correct curvature due to Peyronie’s disease. This involves placing suture opposite the curve in order to straighten the erection. This procedure is done in the operating room. While it is a definitive and effective therapy for many curvatures, it nearly always leads to some penile shortening. Another surgical option is to incise (cut) or excise (remove) the plaque. However, since the plaque exists in the membrane that traps blood in the penis, this produces a gap that must be patched with new tissue in order to keep functioning erections. Often sterilized tissue taken from animal tissues (porcine pericardium) is chosen to plug the defect, but in some cases some loss in erectile function or sensation may result.
Penile Prosthetic Surgery

Inflatable penile prosthetic is a definitive solution that can restore sexual function with men with erectile dysfunction and Peyronie’s disease.
Inflatable penile prosthetic (IPP) placement is a definitive surgical solution to erectile dysfunction and Peyronie’s disease. Normally, the erectile bodies act like elastic “balloons” that fills with blood from the penile arteries in order to distend and create the erection. With the penile prosthetic, the tissue of the erectile bodies is replaced by a plastic “water balloon” that fills with saline (salt water) to create an erection. The device is completely internal and operated using a pump placed next to the testicles inside the scrotum. There are several types of prostheses, with the most advanced types expanding in length and girth and achieving full rigidity after inflation. Since the nerves that supply the penis with sensation are on the outside of the penile, sensation and climax during intercourse is preserved.
For roughly 50% of men with Peyronie’s, the process of placing a IPP alone will lead to satisfactory correction of the curve. When there is minor residual curvature, it can be corrected with manual manipulation in the OR and may improve with repeated use to the IPP over several months to a year. IPP can be an excellent solution for men with both erectile dysfunction and Peyronie’s. Even for men who have erectile dysfunction effectively managed with pills or injections may choose to pursue IPP placement in order to correct curvature that prevents satisfactory intercourse.
Sometimes, it is necessary to combine surgical techniques to correct severe Peyronie’s curves when placing an IPP. Plication or plaque incision/excision can be done together with the placement of the IPP. In some cases, the curve correction is done at the time of initial placement. IPP placement has no impact on urination, sensation, or ejaculation.
Contact Us or email info@mwurology.com with any questions regarding Peyronie’s disease and sexual health treatments.

